Ocular tumors

Description
Ocular tumors are very rare tumors; the most frequent type is retinal melanoma. Sometimes these tumors are located in the conjunctiva (white of the eye) or elsewhere in the orbit.
For the vast majority of these tumors surgery may be avoided. Formerly, the treatment was an eye removal but studies have shown that efficacy results were similar if treated by protontherapy. With this technique, the eye is preserved in 90% of cases with the ability to maintain good vision for many patients
Treatment procedure
Consultation, processing computer simulation, multidisciplinary meeting
Each patient will be seen in consultation by the referring ophthalmologist oncologist to collect all the clinical, radiological and histological information and then present the case in multidisciplinary meeting to validate or not the indication for proton therapy.
Once an indication of protontherapy is validated, metal clips are placed under anesthesia around the tumor. These clips will be very important to allow to always treat the eye in the same position.
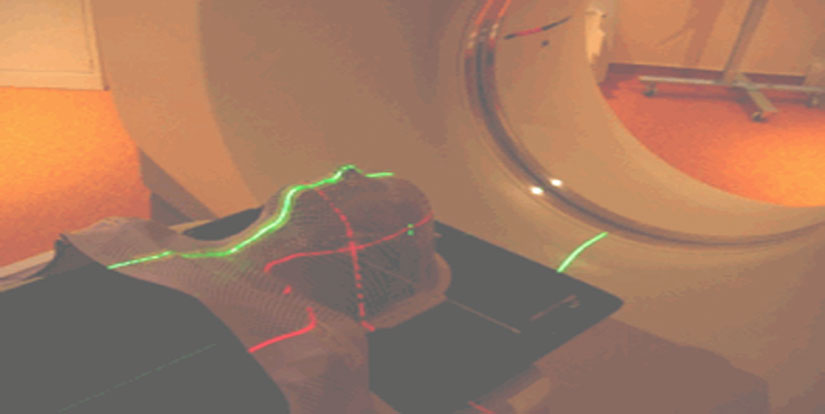
To simulate the treatment, a CT (called “simulation CT”) of the area to be treated will be performed in the treating position. This scanner may require a contrast agent injection. To fully immobilize the treatment area, equipment can be used, such as a plastic mask for head lesions. This is not a diagnostic CT but it collects images that will be used to delineate the treatment area and areas to be avoided by the radiation oncologist. The treatment will then be simulated virtually on a computer-based system to simulate the best beam combinations to better irradiate the tumor while sparing adjacent organs at risk.
Treatment course
Generally for ocular tumors, It only takes 4 treatment sessions on a one per day session basis. Additional training sessions are necessary bringing the total duration of the treatment to 2 weeks.
The irradiation time itself is very short (20 seconds) but it is the time to reposition the patient that takes the most time: you have to put the mask while sitting on a chair, and X-ray images are carried out to see if the metal clips are in the right position. A camera records the eye in real time, allowing to continuously check that the eye remains in position during irradiation.
The eye must fix a small red light at all time to ensure proper positioning.
Side effects
The side effects depend on the treated area and the sensitivity of each, which is not predictable. Some patients will have no side effects, others will. The lists below are not exhaustive and side effects may vary according to size and position of the tumor. These variations are explained by the radiation oncologist during the consultation and the occurrence of side effects can be properly assessed after completion of dosimetry.
The irradiation of eye tumors can be accompanied by the following symptoms:
- in the weeks following irradiation: dry eye sensation (feeling of grains of sand) can rarely cause pain with inflammation / infection of the cornea, depilation of the eyelashes in the months / years after irradiation.
- Appearance of small blood vessels in the eye that can cause small hemorrhages, increased intraocular pressure (neovascular glaucoma) which might rarely result in the need to remove the eye because of too severe pain
- Onset of retina inflammation and especially the area that is responsible for precise vision causing a decrease in visual acuity. The proximity of the tumor with these structures can sometimes lead to complete loss of vision; this vision loss would anyway happen due to tumor progression,
- Clouding of the lens causing cataracts that can be managed in almost all cases by a surgical replacement of the lens by a small prosthesis.

 English
English Deutsch
Deutsch Italiano
Italiano Français
Français Русский
Русский